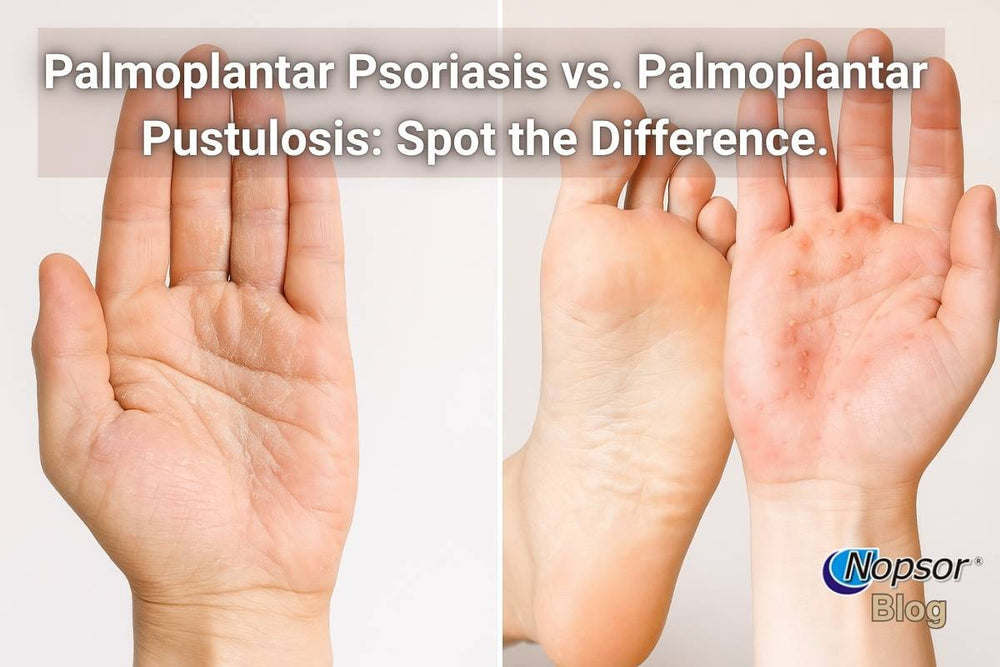
Palmoplantar Psoriasis vs. Palmoplantar Pustulosis: Spot the Difference.
Two Conditions, One Painful Reality: But They're Not the Same
María had been dealing with painful, cracked skin on her hands and feet for months. Some days, tiny blisters filled with pus would appear, making it impossible for her to walk without limping. Her dermatologist initially said it was palmoplantar psoriasis, but after months of treatment with little improvement, another specialist diagnosed her with palmoplantar pustulosis. The change in diagnosis meant a whole new approach to treatment, and for María, a renewed sense of hope.
Stories like María’s are more common than you might think. These two skin conditions share many similarities and can even look almost identical at first glance, but understanding their differences is crucial to getting the right treatment.
Understanding Palmoplantar Psoriasis and Palmoplantar Pustulosis
When skin problems affect the palms of your hands or the soles of your feet, they can impact every part of daily life, from walking and working to simply shaking someone’s hand. Palmoplantar psoriasis (PP) and palmoplantar pustulosis (PPP) are two chronic skin conditions that affect these same areas, causing discomfort, visible changes, and sometimes confusion in diagnosis.
While both involve inflammation, scaling, and irritation, there are key differences in how they look, what causes them, how they progress, and how they respond to treatment. Knowing which one you have can be the difference between months of trial-and-error treatment and a clear path toward relief.
In this guide, we’ll explore the symptoms, causes, diagnosis, and treatment for each condition side by side so you can better understand what’s going on with your skin and work with your healthcare provider to get the right care.
Palmoplantar Psoriasis (PP)
Palmoplantar psoriasis is a localized form of psoriasis that affects the palms and soles. It’s an immune-mediated condition where the skin cell turnover rate speeds up dramatically, leading to thickened, scaly patches.
Typical signs include:
- Thick, rough plaques with a silvery or yellowish scale.
- Painful cracks (fissures) that may bleed or make walking difficult.
- Persistent dryness even with moisturizers.
- A slow, chronic course with periods of flare-ups and remission.
Who gets it?
Palmoplantar psoriasis can affect anyone, but it’s more common in people who already have another form of psoriasis elsewhere on the body.
Triggers and risk factors:
- Stress
- Skin injury or friction
- Cold, dry weather
- Smoking (worsens symptoms)
Palmoplantar Pustulosis (PPP)
Palmoplantar pustulosis is a different condition altogether, despite looking similar to palmoplantar psoriasis. It is characterized by sterile pustules (blisters filled with non-infectious pus) that appear on the palms and soles.
Typical signs include:
- Clusters of small, yellow or white pustules that later turn brown and peel away.
- Red, inflamed skin surrounding the pustules.
- A cyclical pattern where pustules appear, dry out, peel, and return.
- Often more acute flares compared to the slower progression of palmoplantar psoriasis.
Who gets it?
PPP is more common in middle-aged women and has a strong association with smoking.
Triggers and risk factors:
- Tobacco use (major risk factor)
- Stress
- Infections (like tonsillitis)
- Certain medications
Side-by-Side Symptom Comparison Table for Palmoplantar Psoriasis vs. Palmoplantar Pustulosis: Spot the Difference.
Palmoplantar Psoriasis vs. Palmoplantar Pustulosis: Symptom Comparison
Feature |
Palmoplantar Psoriasis (PP) |
Palmoplantar Pustulosis (PPP) |
|
Main Lesion Type |
Thickened, scaly plaques |
Clusters of sterile pustules |
|
Color |
Silvery-white or yellowish scale over red patches |
Yellow/white pustules on a red base |
|
Texture |
Rough, dry, often with deep cracks |
Soft pustules that crust, peel, and recur |
|
Pain & Discomfort |
Pain from deep fissures; tenderness with pressure |
Burning, stinging pain during pustule stage |
|
Itching |
Mild to moderate itching |
Often more intense during pustule flare |
|
Progression Pattern |
Chronic, slow flare-and-remission cycle |
Cyclical pustule eruptions every few weeks |
|
Bleeding |
Common if cracks split open |
Less common; more peeling than bleeding |
|
Associated Symptoms |
May have psoriasis in other body areas (elbows, knees, scalp, nails) |
Usually limited to palms/soles; possible nail changes |
|
Triggers |
Stress, skin trauma, cold/dry weather |
Smoking, infections, stress, certain meds |
How Doctors Diagnose Palmoplantar Psoriasis vs. Palmoplantar Pustulosis
Getting an accurate diagnosis is key because treatments for PP and PPP can differ significantly. While both conditions affect the same areas: palms and soles, doctors look for specific clues during the diagnostic process.
1. Medical History & Symptom Review
PP: Your doctor will ask about personal or family history of psoriasis, flare patterns, and other skin areas involved.
PPP: They may ask about smoking habits, recent respiratory infections, or medications known to trigger pustules.
2. Physical Examination
Lesion type: Thick, scaly plaques point toward PP, while fluid-filled pustules suggest PPP.
Distribution: PP can extend beyond the central palm or sole; PPP tends to be more localized.
3. Skin Biopsy
In unclear cases, a small sample is taken and examined under a microscope.
PP: Shows excessive skin cell growth and inflammation.
PPP: Shows pustules filled with neutrophils (a type of white blood cell).
4. Excluding Other Conditions
Fungal infections (tinea), eczema, and contact dermatitis can mimic these conditions.
Swabs or scrapings may be taken to rule out infections.
5. Nail Examination
Nail pitting or thickening is more common in PP.
PPP may show ridging or discoloration but usually without the classic psoriasis nail changes.
Treatment Differences: Medical and Lifestyle Approaches
While palmoplantar psoriasis (PP) and palmoplantar pustulosis (PPP) share some overlap in symptom management, such as moisturization and trigger avoidance, the core treatment strategies can differ.
Palmoplantar Psoriasis (PP)
Medical Treatments:
· Topical therapies
- Coal tar and salicylic acid (e.g., Nopsor Shampoo & Pomade) to exfoliate thick skin and reduce scaling.
- Topical corticosteroids to reduce inflammation during flares.
- Vitamin D analogs to slow skin cell growth.
Phototherapy:
- Narrowband UVB light can help slow abnormal cell turnover.
Systemic medications:
- Methotrexate, cyclosporine, or biologics for severe, resistant cases.
Lifestyle & Home Care:
- Moisturizing daily with thick creams or ointments, especially after bathing.
- Wearing cotton gloves or socks overnight after applying moisturizers to lock in hydration.
- Avoiding skin trauma, even small cuts can trigger plaques (Koebner effect).
Palmoplantar Pustulosis (PPP)
Medical Treatments:
- Topical corticosteroids, often under occlusion for better absorption.
- Calcipotriol (vitamin D analogs) can be combined with steroids for better effect.
- Phototherapy: PUVA (psoralen plus UVA) can be effective for pustular cycles.
- Systemic medications: Acitretin (oral retinoid) is commonly used; methotrexate or biologics may be considered for stubborn cases.
- Antibiotics: Only if there’s secondary bacterial infection, not for the pustules themselves, which are sterile.
Lifestyle & Home Care:
- Smoking cessation is one of the most critical steps for reducing recurrence.
- Keeping feet and hands cool and dry to prevent irritation.
- Avoiding fragranced soaps and harsh cleansers.
- Using lukewarm soaks with mild emollients to soften peeling skin between flare cycles.
Key Difference in Treatment Philosophy
PP often requires immune-modulating treatments to slow skin cell turnover. PPP treatment focuses more on breaking the pustule cycle and controlling inflammation, with smoking cessation being a cornerstone of care.
Misdiagnosis Risks and Why Clarity Matters
Because palmoplantar psoriasis (PP) and palmoplantar pustulosis (PPP) share many visible traits—redness, scaling, pain, and even some peeling—it’s not uncommon for one to be mistaken for the other, especially in the early stages. But getting it wrong can delay relief for months or even years.
Why Misdiagnosis Happens
- Visual overlap: Early PPP pustules can be small and subtle, looking like pinpoint blisters or scaling spots similar to PP plaques.
- Shared triggers: Stress, skin irritation, and cold weather can worsen both, making it harder to pinpoint the cause.
- Limited awareness: PPP is less common than PP, so some general practitioners may default to a psoriasis diagnosis.
The Cost of the Wrong Diagnosis
Ineffective treatments:
· Someone with PPP might be given coal tar and salicylic acid without addressing smoking, leading to minimal improvement.
· A PP patient misdiagnosed with PPP could be put on acitretin unnecessarily, with avoidable side effects.
Prolonged discomfort: Months of pain, cracked skin, and functional limitations.
Emotional toll: Frustration, anxiety, and the feeling that “nothing works” when in reality, the approach was simply mismatched.
Real-World Insight
On Reddit, one user shared that they lived with “psoriasis” on their feet for two years, using steroid creams that barely helped. A dermatologist later identified PPP and emphasized quitting smoking. Within six months of stopping, their flare cycles shortened dramatically.
Conclusion & Key Takeaways
Palmoplantar psoriasis (PP) and palmoplantar pustulosis (PPP) can look alike, but they don’t behave the same, and they don’t respond to treatment the same way. Getting the name right unlocks the right plan.
Quick recap:
What you see:
- PP: Thick, scaly plaques, deep cracks, slower chronic course.
- PPP: Cycles of small sterile pustules that dry, peel, and return.
What drives it:
- PP: Immune-mediated overgrowth of skin cells.
- PPP: Strong tie to smoking, plus inflammatory flares.
What helps:
- PP: Coal tar, salicylic acid, potent topicals, UVB, and for tough cases, systemic or biologic meds.
- PPP: Potent topicals, PUVA, acitretin or other systemic options, and smoking cessation is often a game-changer.
Diagnosis matters: A dermatologist may use history, exam, and sometimes biopsy to distinguish the two and rule out lookalikes such as fungal infections, eczema, or contact dermatitis.
Next steps if you’re unsure:
Track symptoms (and photos), list triggers, and book a dermatology visit. Ask directly, “Could this be PPP rather than PP?” or vice versa. The goal isn’t a label; it’s the most effective path to relief.
Recommended Reading
-
Palmoplantar Pustulosis vs. Palmoplantar Psoriasis: Spot the Difference
Offers a clear comparison of symptoms, triggers, and treatments—perfect support for understanding the distinctions discussed in the article. -
Best Treatments for Palmoplantar Psoriasis
Delivers an overview of proven therapies such as coal tar, salicylic acid, phototherapy, and systemic options for managing palmoplantar psoriasis. -
Natural Remedies & Lifestyle Tips for Palmoplantar Psoriasis
Shares supportive lifestyle strategies—like moisturizing, stress relief, and diet—that enhance treatment outcomes for palmoplantar skin conditions. -
Living with Palmoplantar Psoriasis: Work, Shoes & Daily Life Tips
Offers practical advice on managing daily activities, footwear, and workplace needs while dealing with hand and foot psoriasis.
References
-
Raposo, I., & Torres, T. (2016). Palmoplantar psoriasis and palmoplantar pustulosis: Current treatment and future prospects. American Journal of Clinical Dermatology, 17, 349–358. Retrieved July 31, 2025, from https://link.springer.com/article/10.1007/s40257-016-0191-7
– Comprehensive review comparing epidemiology, clinical presentation, histopathology, and treatment strategies for PP and PPP. -
DermNet NZ. (2025, April). Palmoplantar pustulosis (localized pustular psoriasis). Retrieved July 31, 2025, from https://dermnetnz.org/topics/palmoplantar-pustulosis/
– Clinical reference outlining differences in presentation, triggers, diagnosis, and treatment outcomes. -
May, B. (2020, September 16). Update on diagnosis and treatment options for palmoplantar pustulosis. Dermatology Advisor. Retrieved July 31, 2025, from https://www.dermatologyadvisor.com/news/updated-diagnosis-and-treatment-options-for-ppp/
– Overview of diagnostic challenges and treatment advances for PPP. -
Patient.info Editorial Group. (2023). Psoriasis of hands and feet (including palmoplantar pustulosis). Patient.info. Retrieved July 31, 2025, from https://patient.info/doctor/psoriasis-of-hands-and-feet-including-palmoplantar-pustulosis
– Doctor-facing resource providing diagnostic and treatment information for palmoplantar psoriasis and PPP.


Leave a comment
Also in Types of Psoriasis
Is It Psoriasis or a Skin Allergy? What to Look For.
August 28, 2025
Red, itchy skin isn’t always what it seems. Many people mistake psoriasis for a simple skin allergy and end up with treatments that don’t work. This guide breaks down the key differences between the two, from what they look like and how they feel to their triggers, duration, and treatments, so you can better understand your skin and know when to see a dermatologist.
Continue reading
Palmoplantar Psoriasis and Psoriatic Arthritis: When Skin and Joints Collide
August 21, 2025
Palmoplantar psoriasis doesn’t just affect the skin, it can also be linked to joint pain and stiffness in the hands and feet, signaling psoriatic arthritis. This article explores the connection between these two conditions, how symptoms overlap, and why early diagnosis is critical. We’ll cover treatment strategies, lifestyle adjustments, and expert insights to help you manage both skin and joint health more effectively.
Continue reading
Psoriasis or Eczema? How to Tell the Difference on Hands and Feet
August 04, 2025
Think you have eczema on your hands or feet? It might actually be psoriasis. This guide breaks down the key differences, real-life stories, and treatment tips to help you get answers and real relief.
Continue reading